The Center for Frugal Innovation at TUHH has initiated an empirical research project to investigate the potential of “affordable and sustainable excellence” in German Healthcare, especially in terms of its potential adoption, likely challenges, and suitable strategies. The project is being carried out in cooperation with the Hochschule Fresenius and builds on our long history of researching frugal innovations in the healthcare sector, see e.g. “Frugal Innovations for a Healthy Society – Learnings for India and Germany”.
Project background
Germany’s healthcare system is well-known for its emphasis on quality, but it also faces mounting and serious challenges to maintain its good performance. Germany’s healthcare spending accounts for 12.6% of its GDP – the highest in European Union (see Figure 1). Due to rising financial burdens, the country has also witnessed closures of hospitals (Niedermann et al., 2025). The number of people in need of long-term care in Germany is projected to increase significantly over the coming years and decades. The ageing population resulting from changing demographic structure of the society is expected to become even more serious in future. Even currently, nearly 40% of citizes aged 65 and over reportedly suffer from more than one chronic condition (OECD, 2023).
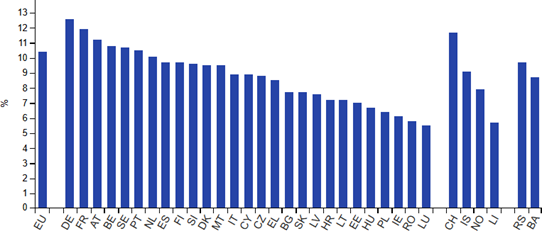
(Source: Eurostat – online data code: hlth_sha11_hf)
Furthermore, Germany faces critical staff shortages with nearly half the practicing physicians being over 50 years of age (Niedermann et al., 2025). As per a survey conducted by Mckinsey & Company, physicians identify staff shortages and bureaucracy as the top challenges (Julius et al., 2024). Germany’s lack of digital adoption in healthcare presents a further challenge (Maass, 2023).
Some examples for Affordable, Sustainable Excellence (ASE)
In the following we list some examples of national healthcare systems and of companies that provide us some insights on how ASE might look like (even if only partially):
- Singapore’s healthcare system: Singapore achieves world-class outcomes while spending less than 4% of GDP on their healthcare (Ministry of Health, 2025). Through smart financing model, digital adoption, personal health responsibility and preventive healthcare strategies,
- India’s healthcare system – Despite the many challenges faced by it, India offers some useful insights for ensuring a good healthcare system. Through process innovations, high volume care, community health workers, and nationwide telemedicine, India has scaled affordable high-quality care at population level (Ramdorai & Herstatt, 2015)
- Many individual companies, such as Siemens Healthineers (e.g. through cost efficient imaging platforms) and GE Healthcare (e.g. through ECG devices) have helped ensure greater accessibility and affordability for excellent-quality medical solutions. Their solutions are often targeted at enabling providers to lower operational costs and improve sustainability.
These examples show how high-quality care can also be achieved without heavy expenditures. These innovations could inform new approaches.
Research objectives
This research project explores how affordable, accessible and effective healthcare solutions can address these challenges in Germany. The research examines, for instance, adoption of globally proven innovations that deliver ‘more with less’, maintaining excellent care and making it affordable through a design shift away from over-engineered solutions and toward a focus on user-centricity. We aim to identify barriers and enablers towards sustainable implementations. By engaging healthcare stakeholders, the study will derive practical strategies to foster these innovations.
Invitation to Engage
We are seeking to interview stakeholders from across the German healthcare ecosystem. We invite inputs, especially in the form of semistructured expert interviews (ca. 30-40 minutes), from healthcare professionals, industry experts, thought leaders, researchers, policymakers, insurers, journalists, patients, solution providers or other interested parties.
Each insight drawn from service receiver to service provider matters.
All contributions will be anonymized, in accordance with the wishes of the interviewed persons, and treated with strict confidentiality.
Project team
Please contact Ms. Somani for further details.
Disclaimer
This research project is not carried out on behalf of any third-party and follows no commercial objectives. Results of the study shall be published and placed in public domain.
References
– Eurostat. (n.d.). Healthcare expenditure statistics – overview. Retrieved from Statistics Explained.
– Julius, C., Wunderlich, E., Wehrmann, J., & Werner, N. (2024, August 12). German healthcare in the postpandemic era: Physician insights.
– Maass, L. (2023). Digital public health in Germany. The European Journal of Public Health, 33 (Supplement 2).
– Ministry of Health. (2025, April 08). Long-term strategies to ensure healthcare cost containment and reduction of unnecessary medical test. Singapore: Ministry of Health.
– Niedermann, F., Deetjen, U., & Rigo, D. (2025, April 02). Future-proofing German healthcare: Three catalysts to accelerate change.
– OECD/European Observatory on Health Systems and Policies. (2023). Germany: Country health profile 2023.
– Ramdorai, A., & Herstatt, C. (2015). Frugal innovation in healthcare: How targeting low-income markets leads to disruptive innovation (1 ed.). Cham: Springer.
– Statistisches Bundesamt. (2023). Number of people in need of long-term care in Germany in 2021 rises to around 4.96 million.
